New Zealand’s aged care system is under significant strain. Our two reviews highlight the need for action to meet the needs of our ageing population.

We were commissioned by Te Whatu Ora to undertake a strategic assessment of the aged care sector in New Zealand and conducted two separate reviews: A Review of Aged Care Funding and Service Models (January 2024) and the Aged Care Service Model and Funding Review: Phase 2 (July 2024). The findings from the first review set the foundation for the second phase of work, which focussed on redesigning funding and services to balance sustainability, quality and affordability. Together, they highlight the urgency of action if the sector is to meet the needs of a rapidly ageing population.
Pressures on the Aged Care Sector
The January 2024 review assessed the current settings for aged residential care (ARC) and home and community support services (HCSS). It found that both parts of the system are underfunded, and that existing funding models are no longer fit for purpose.
- Funding shortfalls: Current regulated prices cover day-to-day operating costs but do not allow for the capital investment needed to build new facilities. Rest home care is the most underfunded, with rural and provincial providers particularly affected.
- Equity concerns: Māori, Pacific, and Asian older people face greater barriers to accessing care. For example, high-priority Māori are admitted to ARC at half the rate of New Zealand European older adults.
- Workforce shortages: Providers in both ARC and HCSS reported difficulty attracting and retaining staff, with wage disparities compared to the hospital sector making the problem worse.
- Strains in HCSS: While public spending on HCSS rose 57% between 2017/18 and 2022/23, the number of clients fell by 7%. This reflects a shift toward more complex clients and higher costs, particularly for travel, which now consumes 18% of the HCSS budget.
Can more support at home reduce ARC demand?
The July 2024 modelling examined whether providing more home-based support could reduce demand for residential care.
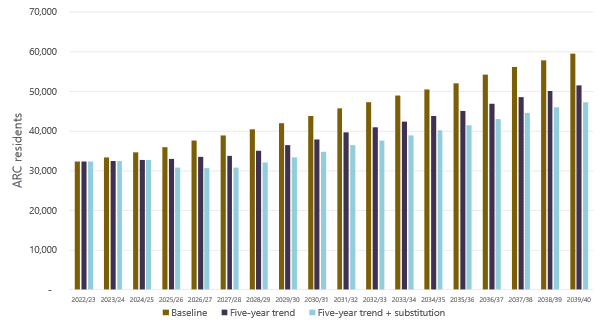
Under the status quo (Baseline scenario), ARC demand is forecast to grow by 84% by 2039/40, reaching about 60,000 residents.
With HCSS substitution, where lower-acuity clients are supported at home, ARC demand would still grow but only by 46%, to about 47,000 residents.
Improving efficiency in HCSS
The July report also considered how adopting a consistent national case-mix model could improve efficiency in HCSS.
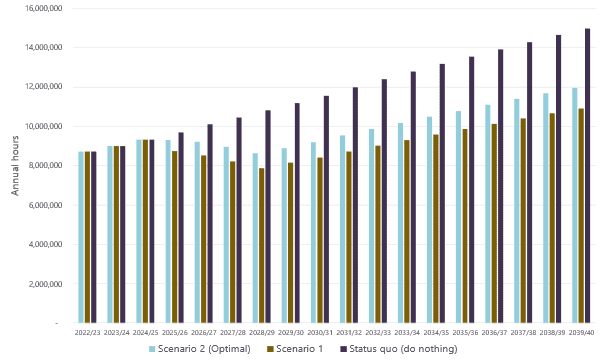
- Under the status quo, HCSS demand is projected to reach 15 million hours annually by 2039/40.
- With case-mix reform, removing lowest-need clients and shifting low-acuity residents from ARC, demand is projected at 11.9 million hours – around 20% lower (Scenario 2 below).
The economics of Aged Residential Care
Financial modelling confirmed that price uplifts are needed across all ARC services to make facilities economically viable.
- For rest home and hospital-level care, uplifts range from 0–3.3% in the base case to 11.9–17.8% in new facility scenarios.
- Regional differences are significant: Auckland and Waitematā require the highest uplifts, largely due to property values.
What Are the Long-Term Fiscal Implications?
The July 2024 modelling compared fiscal costs under current arrangements and alternative funding models for both ARC and HCSS:
- Under the status quo, ARC fiscal costs are forecast at $2.8–3.6 billion annually by 2039/40
- Under an ARC model option that substitutes low-acuity individuals to HCSS and removes maximum subsidies to require higher-income residents to pay unsubsidised fees, costs could be reduced to $1.8–2.3 billion by 2030/40 – a potential saving of over $1 billion annually relative to the status quo
- For HCSS, nationwide adoption of case-mix reform, lower acuity individuals receiving support in HCSS instead of ARC, and lowest need individuals removed from HCSS could generate fiscal savings of around $1.7 billion between 2024/25 and 2039/40.

“Increasing funding alone is not sufficient to generate improved outcomes. While funding models are required for both age residential care and home care support services to incentivise the efficient delivery of services, the system also needs to be designed in a way to enable pathways of care that allow people to live at their desired level of independence.”
Sapere
Time to Act
The two reviews show that New Zealand faces a choice: continue with current settings and accept rising costs, growing inequities, and unmet demand, or implement reforms that shift care toward the home, update funding models, and secure the financial sustainability of the system.
Our team included:
- David Moore
- Jeff Loan
- Rohan Trill
- Mehrnaz Rohani
- Julius Ohrnberger
- Douglas Yee
- Nick Manning
- Lockie Woon
How will your organisation respond to these challenges?
At Sapere, we work with government agencies, providers, and community leaders to analyse funding models, design services, and plan for the future. Our expertise can help you make informed, evidence-based decisions.
Talk to us today about how Sapere can support your organisation in preparing for the future of aged care.
